Status Asthmaticus
Status asthmaticus is a
life-threatening form of asthma in which progressively worsening reactive
airways are unresponsive to usual appropriate therapy that leads to pulmonary
insufficiency. (S. Agarwal, S. Kache.) The primary
mechanical event in status asthmaticus is a progressive increase in airflow
resistance. Mucous plugging and mucosal edema or inflammation is the major
causes for the delayed recovery in status asthmaticus. The combination of hypoxia,
hypercapnia, and acidosis, along with the mechanical effects of increased lung
volumes may result in cardiovascular depression or cardiovascular arrest. (Ibsen)
Causes
- The causes of an acute, severe asthma attack are unknown.
- Poor control of allergens or asthma triggers .
- Infrequently use their peak flow meter and inhaled corticosteroids.
Signs and symptoms
- Cough
- Dyspnea
- Wheezing
- Retractions
- Prolonged expiratory phase
- Pulsus paradoxus - systolic blood pressure drop of more than 18 mmHg with inspiration in teenagers or more than 10 mmHg in children.
- Evidence of cyanosis/hypoxemia - PaO2 less than 60mmHg, change in consciousness.
- Hypercapnia - PaCO2 greater than 40mmHg in presence of dyspnea and wheezing.
- Metabolic acidosis.
- FEV1 or PEFR (peak expiratory flow rate) less than 20% predicted with little or no response to acute therapy
- Silent chest
- Coma
Investigations
1. Vital signs
- Temperature: fever may indicate URI, pneumonia, other source of infection.
- Pulse: Usually tachycardia, even before treatment.
- Respiratory rate: Usually tachypneic.
- . Blood pressure: Pulsus paradoxus over 10-15 correlates well with moderate to severe disease, as it indicates the effect that air trapping is having on the cardiac output.
2. Breath sounds/Chest exam - I:E
ratio is usually 5:2, may be up to 1:4 with a severe attack. The use of
accessory respiratory muscles(abdominal paradoxic breathing, sternocleidomastoid
use, nasal flaring, intercostal retractions) correlates with the severity of
airway obstruction. Feel for the presence of crepitus in the neck or chest
wall, signifying air leak and significant obstruction.
3. Cardiac exam
4. Mental status - Confusion or
obtundation suggest significant hypercapnia or hypoxemia, and necessitate
immediate action.
5. Clinical Asthma Score
6. Pulmonary function tests
7. Chest X-ray
8. Blood gases - Although, blood gases
are often discussed in asthma management, they should not be used to determine
the need for intubation. The patient’s clinical status should be the grounds
for intubation. An attempt at a blood gas often only agitates the patient
further exacerbating the reactive airway process.
Treatment
1. Intravenous Fluids: Patients in SA
are inevitably dehydrated due to poor oral intake, tachypnea, and often emesis.
The dehydration often causes a metabolic acidosis as well increasing their work
of breathing. Rehydration prevents thickening of mucous secretions and begins
to treat the metabolic acidosis.
2. Albuterol: first line therapy
Continuous nebulization - 10-20
mg/hr (or 0.5-0.6 mg/kg/hour) with an oxygen flow rate of 10 – 12L/min.
3. Ipratropium bromide (Atrovent) - 0.25
– 0.5 mg nebulized. Q20 min X 3 doses with continuous albuterol has proven
effective in acute management o Every 6- 8 hrs with Albuterol for chronic
treatment.
4. Corticosteroids – Solu-medrol - Methyl-prednisone
: Loading dose: 2 mg/kg IV o Maintenance dose: 0.5mg/kg IV q 6hr.
( Steroids should be administered IV
to SA patients to assure adequate drug delivery in a timely manner. Given the
risk of emesis and differential absorption enterally, the drug should not be
administered orally.)
5. Magnesium
Sulfate - 50 mg/kg IV over 20 min with max of 2 gm.
6. Terbutaline - Loading dose: 5 -
10mcg/kg IV over 10 min o Continuous infusion: 0.4 - 4 mcg/kg/min IV.
7. Mechanical
ventilation - Start with low tidal volume, permissive hypercapnia strategy.
1. Tidal volume 4-7 ml/kg (prevents barotrauma /
volutrauma, minimize lung distension).
2. Low Ventilatory rate 10-14 breaths per minute.
3. I:E ratio 1:4 to 1:6 (avoid air trapping by
allowing for complete exhalation).
4. Tolerate hypercapnia.
5. Goal pH>7.25 (may require HCO3) .
6. Peak pressures.
( http://www.youtube.com/watch?v=Px42rbK8fIo )
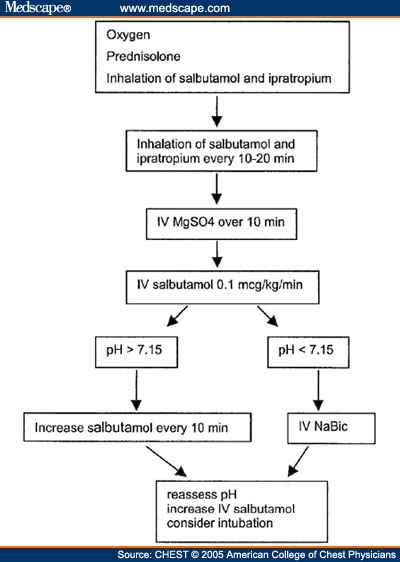
( http://img.medscape.com/fullsize/migrated/501/434/ch501434.fig1.jpg )
( http://www.samj.org.za/index.php/samj/article/viewFile/6526/5004/34638 )
References
- Anonymous. (2024). Asthma guide. Retrieved April 28, 2015, from web med: http://www.webmd.boots.com/asthma/guide/status-asthmaticus.
- Ibsen, L. (n.d.). Status Asthmaticus. Retrieved April 28, 2015, from pedsccm.org: http://pedsccm.org/FILE-CABINET/Practical/Akron_pdfs/7ASTHMAP.PDF.
- S. Agarwal, S. Kache. (n.d.). STATUS ASTHMATICUS. Retrieved April 28, 2015, from peds.stanford.edu: http://peds.stanford.edu/Rotations/picu/pdfs/14_status_asthmaticus.pdf.
- S.A.Papiris , E.D.Manali , L. Kolilekas,C. Triantafillidou , I.Tsangaris . (2009). Acute severe asthma: new approaches to assessment and treatment. Retrieved April 28, 2015, from pub med: http://www.ncbi.nlm.nih.gov/pubmed/19911854

No comments:
Post a Comment