Acute Myocardial Infarction
Causes for MI
Acute
myocardial infarction is thus defined as myocardial necrosis due to prolonged
myocardial ischemia ( Toraih, E., Hussein,
M. H., & Badran, D. I. 2014). Critical myocardial ischemia can occur as a result of
increased myocardial metabolic demand, decreased delivery of oxygen and
nutrients to the myocardium via the coronary circulation, or both. An
interruption in the supply of myocardial oxygen and nutrients occurs when a
thrombus is superimposed on an ulcerated or unstable atherosclerotic plaque and
results in coronary occlusion. A high-grade (>75%) fixed coronary artery
stenosis caused by atherosclerosis or a dynamic stenosis associated with
coronary vasospasm can also limit the supply of oxygen and nutrients and
precipitate an MI. (H. M. Bolooki , A. Askari. 2010)
Risk factors.
Established risk factors
- Raised plasma low density lipoprotein cholesterol
- Decreased plasma high density lipoprotein cholesterol
- Smoking
- High blood pressure
- Increased plasma glucose concentrations
- Physical inactivity
- Obesity
- Advanced age
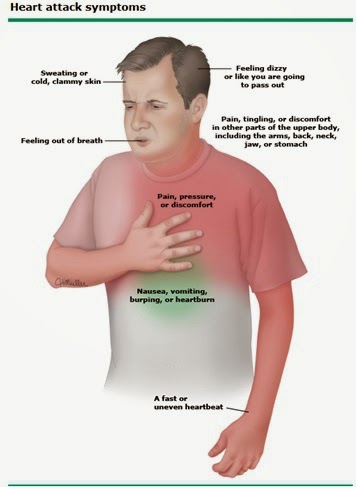
- There are two sets of sings and symptoms for acute myocardial infarction. there are,
- Cardio respiratory arrest.
- Angina pectoris.
Sings and Symptoms of,
Cardio respiratory arrest.- Breathlessness
- Absent pulse.
- Loss of consciousness.
Angina Pectoris.
- Crushing chest pain which may radiating to neck, jaw or one or both arms.
- Anxiety.
- Dyspnoea.
- Faintness.
- Nausea.
- Shortness of breath.
- Sweating or cold skin.
- Pallor.
- Rapid or irregular heartbeat.
- Fatigue.
- Dizziness.
 |
Ideal cure, myocardial infarction, 7.09.2014,http://ktthebest4u.blogspot.com/2014/09/myocardial-infarction.html |
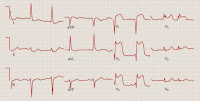 |
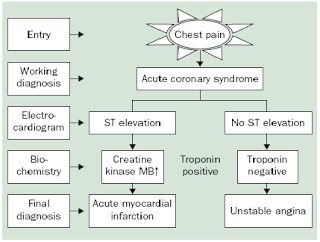
| ST elevation MI |
(http://www.clevelandclinicmeded.com/medicalpubs/diseasemanagement/cardiology/acute-myocardial-infarction/images/amifig1_large.jpg)
Non-ST elevation MI
2. Laboratory tests
- Cardiac biomarkers/enzymes
· Troponin levels: Troponin is a contractile protein that normally is not found in serum; it is released only when myocardial necrosis occurs.
· Creatine kinase (CK) levels: CK-MB levels increase within 3-12 hours of the onset of chest pain, reach peak values within 24 hours, and return to baseline after 48-72 hours.
· Myoglobin levels: Myoglobin is released more rapidly from infarcted myocardium than is troponin; urine myoglobin levels rise within 1-4 hours from the onset of chest pain.
Timing of release of cardiac serum markers after acute ischaemic myocardial infarction
2. Complete blood count
3. Chemistry profile
2. Laboratory tests
· Troponin levels: Troponin is a contractile protein that normally is not found in serum; it is released only when myocardial necrosis occurs.
· Creatine kinase (CK) levels: CK-MB levels increase within 3-12 hours of the onset of chest pain, reach peak values within 24 hours, and return to baseline after 48-72 hours.
· Myoglobin levels: Myoglobin is released more rapidly from infarcted myocardium than is troponin; urine myoglobin levels rise within 1-4 hours from the onset of chest pain.
Timing of release of cardiac serum markers after acute ischaemic myocardial infarction
2. Complete blood count
3. Chemistry profile
4. Lipid profile
5. C-reactive protein and other inflammation markers
3. Cardiac imaging - For individuals with highly probable or confirmed MI, a coronary angiogram can be used to definitively diagnose or rule out coronary artery disease. ( A.M.Zafari, E.H.Yang, 2015)
Coronary Angiogram.
Diagnosis of MI.
( http://www.siumed.edu/medicine/cardiology/cardiorotation/articles/Acute%20Myocardial%20Infarction.pdf )
( http://www.siumed.edu/medicine/cardiology/cardiorotation/articles/Acute%20Myocardial%20Infarction.pdf )
Management
Prehospital care
· Intravenous access, supplemental oxygen, pulse oximetry
· Immediate administration of aspirin en route
· Nitroglycerin for active chest pain, given sublingually or by spray
Emergency department
- CPR – Cardiopulmonary resuscitation for symptom of cardio respiratory arrest.
( http://www.youtube.com/embed/r8iU3Mtblho?controls=0&rel=0&showinfo=0&wmode=transparent )
- Initial stabilization of patients with suspected myocardial infarction and ongoing acute chest pain should include administration of sub lingual nitroglycerin if patients have no contraindications to it.
- The American Heart Association (AHA) recommends the initiation of beta blockers to all patients with STEMI (unless beta blockers are contraindicated).
- If STEMI is present, the decision must be made quickly as to whether the patient should be treated with thrombolysis or with primary per cutaneous coronary intervention (PCI).
- Although patients presenting with no ST-segment elevation are not candidates for immediate thrombolytics, they should receive anti-ischemic therapy and may be candidates for PCI urgently or during admission.
Emergency department
Pharmacological Treatment
1. Anti platelet Medications
The use of aspirin has been shown to reduce mortality
from MI. Aspirin in a dose of 325 mg should be administered immediately on
recognition of MI signs and symptoms.
2. Supplemental Oxygen.
Oxygen should be administered to patients with symptoms
or signs of pulmonary edema or with pulse oximetry less than 90% saturation.
The rationale for using oxygen is the assurance that erythrocytes will be
saturated to maximum carrying capacity. Because MI impairs the circulatory
function of the heart, oxygen extraction by the heart and by other tissues may
be diminished. In some cases, elevated pulmonary capillary pressure and
pulmonary edema can decrease oxygen uptake as a result of impaired pulmonary
alveolar-capillary diffusion.
3. Nitrates
Intravenous
nitrates should be administered to patients with MI and congestive heart
failure, persistent ischemia, hypertension, or large anterior wall MI. The primary benefit of nitrates is derived from its
vasodilator effect. Nitrates are metabolized to nitric oxide in the vascular
endothelium. Nitric oxide relaxes vascular smooth muscle and dilates the blood
vessel lumen. Vasodilatation reduces cardiac preload and after load and
decreases the myocardial oxygen requirements needed for circulation at a fixed flow rate. Vasodilatation of the
coronary arteries improves blood flow through the partially obstructed vessels
as well as through collateral vessels. Nitrates can reverse the
vasoconstriction associated with thrombosis and coronary occlusion. ( A.M.Zafari, E.H.Yang, 2015)
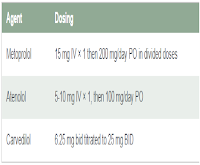
4.
Beta Blockers
5. ACE Inhibitors
6. Unfractionated Heparin
Unfractionated heparin is beneficial until the inciting
thrombotic cause (ruptured plaque) has completely resolved or healed.
Unfractionated heparin has been shown to be effective when administered
intravenously or subcutaneously according to specific guidelines. The minimum
duration of heparin therapy after MI is generally 48 hours, but it may be
longer, depending on the individual clinical scenario.
7. Low-Molecular-Weight Heparin
Low-molecular-weight
heparin (LMWH) can be administered to MI patients who are not treated with
fibrinolytic therapy and who have no contraindications to heparin. The LMWH
class of drugs includes several agents that have distinctly different
anticoagulant effects.
8. Warfarin
Warfarin
is not routinely used after MI, but it does have a role in selected clinical
settings. The latest guidelines recommend the use of warfarin for at least 3
months in patients with left ventricular aneurysm or thrombus, a left
ventricular ejection fraction less than 30%, or chronic atrial fibrillation.
Surgical Revascularization
Emergent or urgent coronary artery bypass grafting (CABG) is
warranted in the setting of failed PCI in patients with hemodynamic instability
and coronary anatomy amenable to surgical grafting.
REFERENCES
- Toraih, E., Hussein, M. H., & Badran, D. I. Beta 2-Adrenergic Receptor Gene Polymorphisms in Egyptian Patients with Acute Myocardial Infarction.Advances in Molecular Biology, 2014.
- H. M. Bolooki , A. Askari. Acute Myocardial Infarction, Cleveland clinic,2010, Aug. http://www.clevelandclinicmeded.com/medicalpubs/diseasemanagement/cardiology/acute-myocardial-infarction/Default.htm.
- E.Boersma, N.Mercado, D.Poldermans, M.Gardien, J.Vos, M.L.Simoons. (2003, March 08). Acute myocardial infarction. Retrieved April 28, 2015, from http://www.siumed.edu/: http://www.siumed.edu/medicine/cardiology/cardiorotation/articles/Acute%20Myocardial%20Infarction.pdf.
- A.M.Zafari, E.H.Yang. (2015, April 1). Myocardial Infarction . Retrieved April 28, 2015, from medscape.com: http://emedicine.medscape.com/article/155919-overview

.jpg)